|
Treating the disease, osteoporosis, earlier is vital to increase survival and quality of life.
Knowing these facts, survivors need to have osteoporosis evaluation.
- Facts:
- 1. Common disease with aging
2. Most common in post menopausal women
3. Common in men treated with androgen deprivation therapy (ADT) for prostate cancer and women treated with chemotherapy for breast cancer
Osteoporosis is a disease that involves severe thinning of bone that can lead to weak and fragile bones. People with osteoporosis are at risk for fractures (broken bones), particularly in the hip, spine, and wrist. This is a common problem among postmenopausal women and patients who survive cancer and its therapy, especially in women who receive chemotherapy for breast cancer and men with prostate cancer receiving hormone deprivation therapy.
Premenopausal women, when treated with chemotherapy, are at greater risk for osteopenia (a term for mildly reduced bone mass) and osteoporosis due to ovarian failure (with accompanying low levels of estrogen) following cancer therapy.
What Causes Osteoporosis?
Back to the Table of Contents
 Most people consider it natural that our bones grow weak with age. Peak bone strength is reached at an age of about 25 years, and there is gradual loss of bone after that age. To understand the causes of osteoporosis, one must understand that normal bones are constantly in a process involving bone formation (where bone is being built up) and resorption (where bone is being broken down).
Osteoporosis occurs when an imbalance occurs between new bone formation and old bone resorption, with more bone resorbed than formed. Calcium and vitamin D are very important in promoting bone formation, and a diet deficient in calcium and vitamin D can lead to a low amount of bone formation, resulting in bone loss. Weight-bearing exercise also helps bone formation, and people who do not participate in such exercise can lose bone as well. A long-term diet rich in calcium and vitamin D supplements and a weight-bearing exercise program designed to promote and maintain bone strength may help to prevent the bone loss that begins in middle age. Changes in hormones with age lead to bone loss as well. Low estrogen levels in women, as found in women after menopause or in premenopausal women after surgery to remove the ovaries (called oophorectomy) leads to more rapid bone resorption and loss. In fact, the leading cause of osteoporosis in women is a lack of the hormone estrogen. Inadequate dietary calcium (< 1200 mg per day) and vitamin D supplements, insufficient weight-bearing exercise, and natural loss of hormones can cause bones to become porous, brittle, and, ultimately, to fracture with minimal trauma. In men, the male hormone testosterone also helps maintain bone strength, and low levels can lead to bone loss as well. Although testosterone levels decline naturally in men with age, the effect of this minor change in testosterone levels on osteoporosis is not clear.
Most people consider it natural that our bones grow weak with age. Peak bone strength is reached at an age of about 25 years, and there is gradual loss of bone after that age. To understand the causes of osteoporosis, one must understand that normal bones are constantly in a process involving bone formation (where bone is being built up) and resorption (where bone is being broken down).
Osteoporosis occurs when an imbalance occurs between new bone formation and old bone resorption, with more bone resorbed than formed. Calcium and vitamin D are very important in promoting bone formation, and a diet deficient in calcium and vitamin D can lead to a low amount of bone formation, resulting in bone loss. Weight-bearing exercise also helps bone formation, and people who do not participate in such exercise can lose bone as well. A long-term diet rich in calcium and vitamin D supplements and a weight-bearing exercise program designed to promote and maintain bone strength may help to prevent the bone loss that begins in middle age. Changes in hormones with age lead to bone loss as well. Low estrogen levels in women, as found in women after menopause or in premenopausal women after surgery to remove the ovaries (called oophorectomy) leads to more rapid bone resorption and loss. In fact, the leading cause of osteoporosis in women is a lack of the hormone estrogen. Inadequate dietary calcium (< 1200 mg per day) and vitamin D supplements, insufficient weight-bearing exercise, and natural loss of hormones can cause bones to become porous, brittle, and, ultimately, to fracture with minimal trauma. In men, the male hormone testosterone also helps maintain bone strength, and low levels can lead to bone loss as well. Although testosterone levels decline naturally in men with age, the effect of this minor change in testosterone levels on osteoporosis is not clear.
- Aside from age, other risk factors in women include:
- 1. Being postmenopausal
2. Being female
3. Being chronically underweight
4. Being Caucasian or Asian
5. Past history of scant or prolonged absence of periods (amenorrhea)
6. Having a family history of osteoporosis
7. A poor diet lacking minerals, especially calcium
8. Being sedentary
9. Lack of weight-bearing exercise
10. Smoking, drinking alcohol in excess, taking excess caffeine, and certain drugs such as cortisone (prednisone, hydrocortisone, dexamethasone), thyroid hormone, and anti-convulsants
-
Osteoporosis is most common in women, but occurs in men as well. The major risk factors in men include age > 70 years, low body weight, physical inactivity, cigarette smoking, low calcium and vitamin D intake, prolonged steroid use, gastrointestinal malabsorption, and low bone density.
How Common is Osteoporosis?
Back to the Table of Contents
Osteoporosis is responsible for more than 1.5 million fractures annually, mostly of the hip, spine, and wrist. 10 million Americans already have osteoporosis and 34 million more have a low bone mass (osteopenia), placing them at increased risk for osteoporosis. Eighty percent of those with osteoporosis are women after the menopause. It is called a silent disease, because it takes many years to develop, and most sufferers do not learn that they have the disease until middle age or later, and, often, not until after a fracture has occurred. There are usually no symptoms associated with osteoporosis: the first symptom could be a fracture. It commonly afflicts menopausal women. Osteoporosis usually occurs much later in life and affects both sexes.
One out of every two women (50%) and one in four men (25%) over age 50 will have an osteoporosis-related bone fracture in their lifetime. After age 80, 5% of women will have a hip fracture, and 20% of these people will then die within a year. Forty thousand people will die each year of complications following osteoporosis-associated fractures. The annual medical costs associated with osteoporosis totals between 14 and 18 billion dollars. Thus, osteoporosis and its complications have both a personal and an economic impact.
How Do You Find Out If You Have Osteoporosis?
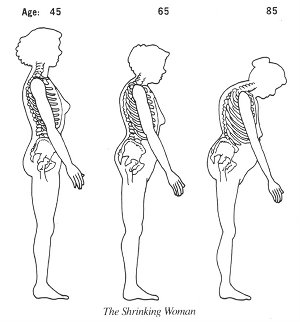
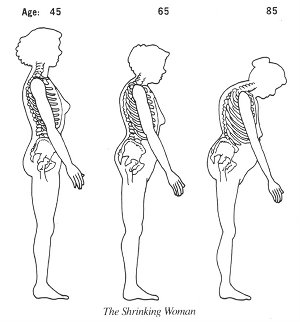
Routine x-rays and blood and urine tests are not adequate in looking for osteoporosis. Loss of height and development of so-called dowager's hump (an outward curvature of the upper back due to compression fractures of the front portions of the vertebra) are late findings. It is possible to discover bone loss early by the use of Dual Energy X-ray Absorptiometry (DEXA or DXA), which can accurately and rapidly measure bone mineral content at the wrist, the spine and the hip with little discomfort and at reasonable cost with minimal exposure to x-rays. The result of the bone density test is a number which is compared to a normal result for someone of similar age, sex and size. This information will tell the doctor how your bone strength compares to others in your age group. The result of the test can also be compared to the average bone strength of a healthy young adult. Both of these comparisons give the doctor important information regarding how the bone strength compares to others. Mildly low bone density can reflect osteopenia, or mild to moderate bone loss. Lower bone density leads to a diagnosis of osteoporosis. The results of the bone density test can also give information on the potential risk for having a fracture.
What Can Be Done to Treat Osteoporosis?
Back to the Table of Contents
-
Once a diagnosis of osteoporosis is made, the treatment is focused on ways of slowing down if not stopping the bone loss, increasing bone strength, preventing fractures, and helping the pain that may happen with fractures.
-
Lifestyle modifications including regular exercise are important to prevent bone loss and lead to stronger bones. This exercise should be weight bearing, and such exercises include walking, weight lifting, riding stationary bicycles, jogging, and using a rowing machine. Swimming, although an excellent exercise, is non-weight bearing and would not be useful for preventing or treating osteoporosis.
Dietary Therapy: A long-term diet rich in calcium and vitamin D supplements may help to offset the bone loss that begins in middle age.
Recommendations for dietary calcium: A daily calcium intake of 1200-1500 mg (through dietary products and supplements) is recommended. Calcium supplements come in various doses, but doses should not be more than about 600 mg at a time, as the body cannot absorb more than that per dose. Therefore, the doses should be split up during the day. See Table 1 for foods and drinks that contain calcium. For calcium supplements, there are two types of calcium tablets: calcium carbonate and calcium citrate. Because calcium citrate is absorbed better in patients with low acid content in the stomach (such as in patients taking H2 blockers (e.g., Zantac®, Tagamet®) or proton pump inhibitors, calcium citrate is usually recommended as a first line calcium supplement in patients who are on such medications. Otherwise, calcium carbonate is generally recommended as first-line therapy, and calcium carbonate should be taken with meals.
| Foods and Drinks with Calcium |
| Food |
Calcium, milligrams |
| Milk (skim, 2 percent, or whole, 8 oz)
|
300 |
| Yogurt (6 oz)
|
250 |
| Orange Juice (with calcium, 8 oz)
|
300 |
| Tofu with calcium (1/2 cup)
|
435 |
| Cheese (1 oz) (hard cheese = higher calcium)
|
195-335 |
| Cottage cheese (1/2 cup)
|
130 |
| Ice cream or frozen yogurt (1/2 cup)
|
100 |
| Soy milk (1 cup)
|
100 |
| Beans (1/2 cup cooked)
|
60-80 |
| Sardines (one)
|
92 |
| Canned salmon (3 oz)
|
185 |
| Tuna, canned (3 oz)
|
10 |
|
Dark, leafy green vegetables (1/2 cup cooked)
|
50-135 |
| Dried figs (3)
|
80 |
| Almonds (24 whole)
|
70 |
| Orange (1 medium)
|
70 |
Recommendations for dietary Vitamin D: Daily intake of 400-800 IU of vitamin D (via foods or supplements) is needed to maintain bone mass, and 800-1,000 IU of vitamin D per day is recommended to increase bone mass in people with osteoporosis. Very few foods in nature contain vitamin D. Fish (such as salmon, tuna, and mackerel) and fish liver oils are among the best sources (200-360 IU per serving). One cup of milk, whether nonfat, low fat, or whole, contains 100 IU of vitamin D. Swiss cheese contains only 12 IU per ounce. A standard multivitamin tablet contains 400 IU of vitamin D, so one to two multivitamin tablets a day will result in an adequate intake of vitamin D.
There are two forms of vitamin D, Vitamin D2 (ergocalciferol ) and Vitamin D3 (cholecalciferol). Vitamin D3 is a highly active form of vitamin D and previous studies suggested that vitamin D3 was a better choice than vitamin D2. However, more recent studies show that vitamin D3 and vitamin D2 are equally good for bone health.
Medical Therapy
Back to the Table of Contents
For menopausal women, estrogen therapy can prevent bone loss and lead to an increase in bone strength. A concern with regard to estrogen involves recent studies that question the safety of long-term estrogen use, including the increased risk for developing breast cancer, heart disease, and stroke. Therefore, estrogen therapy has a more limited role these days in the treatment of osteoporosis.
Bisphosphonates are medications that reduce bone loss, leading, in many cases, to an increase in bone strength. These medications include Alendronate (Fosamax®), Risendronate (Actonel®), and Ibandronate (Boniva®). These are oral medications that can improve bone strength and help prevent fractures. Side effects of these medications include stomach upset. These medications are oral. Zoledronic Acid (Zometa®) is an intravenous bisphosphonate used to treat osteoporosis. This is given once a year for the treatment of osteoporosis. A rare but serious side effect of the bisphosphonates is osteonecrosis (bone breakdown) of the jaw. Risk factors for osteonecrosis of the jaw includes dental work involving the bone of the jaw or simultaneous use of steroid medications.
Teriparatide (Forteo®): This is a medication that contains a portion of human parathyroid hormone and may lead to new bone formation and increased bone strength. This drug is given as a daily subcutaneous injection.
-
Osteoporosis in Patients with Breast and Prostate Cancer
-
Osteopenia and osteoporosis are common problems associated with age and cancer survivorship. In most cases, breast and prostate cancer survivors have strong skeletons before treatment, and then lose bone with cancer related therapy. Such survivors should follow a calcium rich diet with calcium supplements and vitamin D, exercise as tolerated, as well as seek guidance from their healthcare providers for possible use of drug treatment which can increase bone strength.
- Osteoporosis and Breast Cancer Endocrine Therapy
- The original treatment for metastatic breast cancer (1898) was surgical oophorectomy (removal of the ovaries) or later in the 1900's radiation ablation (loss of function) of the ovaries to stop estrogen production.
Adjuvant and therapeutic chemotherapy, radiotherapy, or hormonal ablation can also reduce or stop ovarian function, and reduce or stop estrogen production. This can result in premature bone loss. Adjuvant use of selective estrogen-receptor modulators (SERMS, see below) can help improve overall and disease-free survival but are less effective than the selective aromatase inhibitors. Although SERMS are effective breast cancer treatments because they block estrogens, they also have some protective effect on bone density (by increasing the estrogen effect on bone, different from the effect on the breast). The ability of SERMS to protect bone is greater in postmenopausal rather than in premenopausal women.
- Osteoporosis and the Selective Estrogen-Receptor Modulators for Breast Cancer
- Another drug class is that of the selective estrogen-receptor modulators (SERMs). Evista (Raloxifene®) and Nolvadex (Tamoxifen®) act as estrogen antagonists against hormone positive breast cancer and can help reduce the risk of invasive breast cancer. The FDA Oncology Drug Advisory Committee (ODAC/ Aug 2007) in NCI Bulletin recommended approval of Raloxifene to prevent breast cancer in women with osteoporosis based on results from 4 studies, including the pivotal STAR trial which showed Raloxifene was as effective as Tamoxifen in reducing the breast cancer risk (prevention) in postmenopausal women. The STAR trial showed Raloxifene and Tamoxifen reduced the risk of invasive breast cancer approximately 50 %. Raloxifene had a better safety profile with fewer blood clots, endometrial cancer and cataracts (similar to estrogen). Both Raloxifene and Tamoxifen help reduce the risk of osteoporosis by having an estrogen-like effect on bone. Raloxifene (Evista®) is approved by the FDA to prevent and treat osteoporosis in postmenopausal women.
- Osteoporosis and the Selective Aromatase Inhibitors for Breast Cancer
- Selective aromatase inhibitors are a recent class of drugs for postmenopausal patients for adjuvant as well as metastatic breast cancer therapy. These drugs work by lowering levels of estrogen in the body. The three types of aromatase inhibitor drugs - anastrozole (Arimidex®) and letrozole (Femara®) are non-steroidal, and exemestane (Aromasin®) are steroidal drugs that irreversibly inhibit the aromatase enzyme, causing low estrogen levels. By lowering estrogen levels, these drugs increase bone resorption, leading to loss of bone strength.
- Osteoporosis and Prostate Cancer
- One of the major treatments of male prostate cancer involves reducing the male hormone testosterone to extremely low levels (hormone ablation treatment). Hormone ablation treatment (also called androgen deprivation therapy or ADT) can be performed by either injectible hormone treatment (GnRH agonist - Lupron® or Zoladex®) or orchiectomy (surgical removal of testicles). Following androgen hormone ablation treatment, patients with prostate cancer may develop osteoporosis within as short a period as 6 months to two years due to a decrease in blood levels of testosterone. Osteoporotic skeletal fractures can occur in up to 20% of men within 5 years of starting ADT. Treatment for osteoporosis/osteopenia is the same as for breast cancer (diet, calcium, Vitamin D, weight-bearing exercises, and bisphosphonates [such as the injectible bisphosphonates Zometa® or Aredia®] as needed to help prevent bone loss.)
- Cancer, Osteoporosis, and Bone Density Treatment for Metastases
- Bone metastases from breast or prostate cancer are common. Bone resorption is accelerated, leading to an increased vertebral, hip and wrist bone fracture rate. Treatment for osteoporosis/osteopenia includes diet, calcium, Vitamin D, exercise (with caution to avoid a bone fracture) and bisphosphonates [Zometa® or Pamidronate®] to protect bones from the reabsorptive activity of cancer metastases.
- Summary
- Bone loss is a common finding in patients with breast and prostate cancer. Prevention of osteoporosis is key, and interventions such as proper diet, exercise and other lifestyle modifications will help prevent bone loss. Proper diagnostic tests should be performed to determine bone strength, and use of medications that improve bone strength may be necessary to prevent osteoporosis and fractures.
|
|

 Most people consider it natural that our bones grow weak with age. Peak bone strength is reached at an age of about 25 years, and there is gradual loss of bone after that age. To understand the causes of osteoporosis, one must understand that normal bones are constantly in a process involving bone formation (where bone is being built up) and resorption (where bone is being broken down).
Osteoporosis occurs when an imbalance occurs between new bone formation and old bone resorption, with more bone resorbed than formed. Calcium and vitamin D are very important in promoting bone formation, and a diet deficient in calcium and vitamin D can lead to a low amount of bone formation, resulting in bone loss. Weight-bearing exercise also helps bone formation, and people who do not participate in such exercise can lose bone as well. A long-term diet rich in calcium and vitamin D supplements and a weight-bearing exercise program designed to promote and maintain bone strength may help to prevent the bone loss that begins in middle age. Changes in hormones with age lead to bone loss as well. Low estrogen levels in women, as found in women after menopause or in premenopausal women after surgery to remove the ovaries (called oophorectomy) leads to more rapid bone resorption and loss. In fact, the leading cause of osteoporosis in women is a lack of the hormone estrogen. Inadequate dietary calcium (< 1200 mg per day) and vitamin D supplements, insufficient weight-bearing exercise, and natural loss of hormones can cause bones to become porous, brittle, and, ultimately, to fracture with minimal trauma. In men, the male hormone testosterone also helps maintain bone strength, and low levels can lead to bone loss as well. Although testosterone levels decline naturally in men with age, the effect of this minor change in testosterone levels on osteoporosis is not clear.
Most people consider it natural that our bones grow weak with age. Peak bone strength is reached at an age of about 25 years, and there is gradual loss of bone after that age. To understand the causes of osteoporosis, one must understand that normal bones are constantly in a process involving bone formation (where bone is being built up) and resorption (where bone is being broken down).
Osteoporosis occurs when an imbalance occurs between new bone formation and old bone resorption, with more bone resorbed than formed. Calcium and vitamin D are very important in promoting bone formation, and a diet deficient in calcium and vitamin D can lead to a low amount of bone formation, resulting in bone loss. Weight-bearing exercise also helps bone formation, and people who do not participate in such exercise can lose bone as well. A long-term diet rich in calcium and vitamin D supplements and a weight-bearing exercise program designed to promote and maintain bone strength may help to prevent the bone loss that begins in middle age. Changes in hormones with age lead to bone loss as well. Low estrogen levels in women, as found in women after menopause or in premenopausal women after surgery to remove the ovaries (called oophorectomy) leads to more rapid bone resorption and loss. In fact, the leading cause of osteoporosis in women is a lack of the hormone estrogen. Inadequate dietary calcium (< 1200 mg per day) and vitamin D supplements, insufficient weight-bearing exercise, and natural loss of hormones can cause bones to become porous, brittle, and, ultimately, to fracture with minimal trauma. In men, the male hormone testosterone also helps maintain bone strength, and low levels can lead to bone loss as well. Although testosterone levels decline naturally in men with age, the effect of this minor change in testosterone levels on osteoporosis is not clear.